May 2021 is Lupus Awareness Month
Lupus is the Latin word for wolf. 13th century physician Rogerius used it to describe erosive facial lesions that were reminiscent of a wolf’s bite, one of the manifestations of the auto-immune disease we call Lupus. Every year there are monthly health awareness observances. These observances help us all learn to be aware, proactive and responsible for our own health and those of our loved ones. May is traditionally a time of renewal with spring planting, flowers, yard work and that all important Hallmark holiday which is Mother’s Day. May is also important to those who live with Lupus.
Lupus is a chronic, auto-immune disease, meaning it attacks the host body’s organs and tissues. In laymen’s terms this means the immune system we all depend on as our first line of defense against illness is working against us. The anti-inflammatory mechanisms have backfired, and this inflammation can run amok. Lupus is often localized in joints, skin or internal organs (heart, lungs, skin, kidneys) but as with any issues of inflammation, it can manifest itself just about anywhere. Adding to the ambiguity is the fact that symptoms can appear suddenly, flare up occasionally, disappear entirely or any combination thereof. It is not contagious and not necessarily inherited. Most of the difficulty in diagnosing and/or treating Lupus is in the individualized nature of the disease.
Causes of Lupus
Most of us are hardwired to know the ‘why’ of things. With Lupus, we are not able to get a definitive answer. Links have been found to environment and lifestyle decisions like nicotine use/exposure, stress or even silica dust. 50 genes have been identified as posing an elevated risk of Lupus, especially when accompanied by a family history. Elevated levels of estrogen have been linked. Infections like Epstein-Barr (a type of herpes virus) or cytomegalovirus (associated with mononucleosis) can also mimic Lupus. There is also evidence that long term use of medications used for irregular heart rhythms and high blood pressure can trigger Lupus.
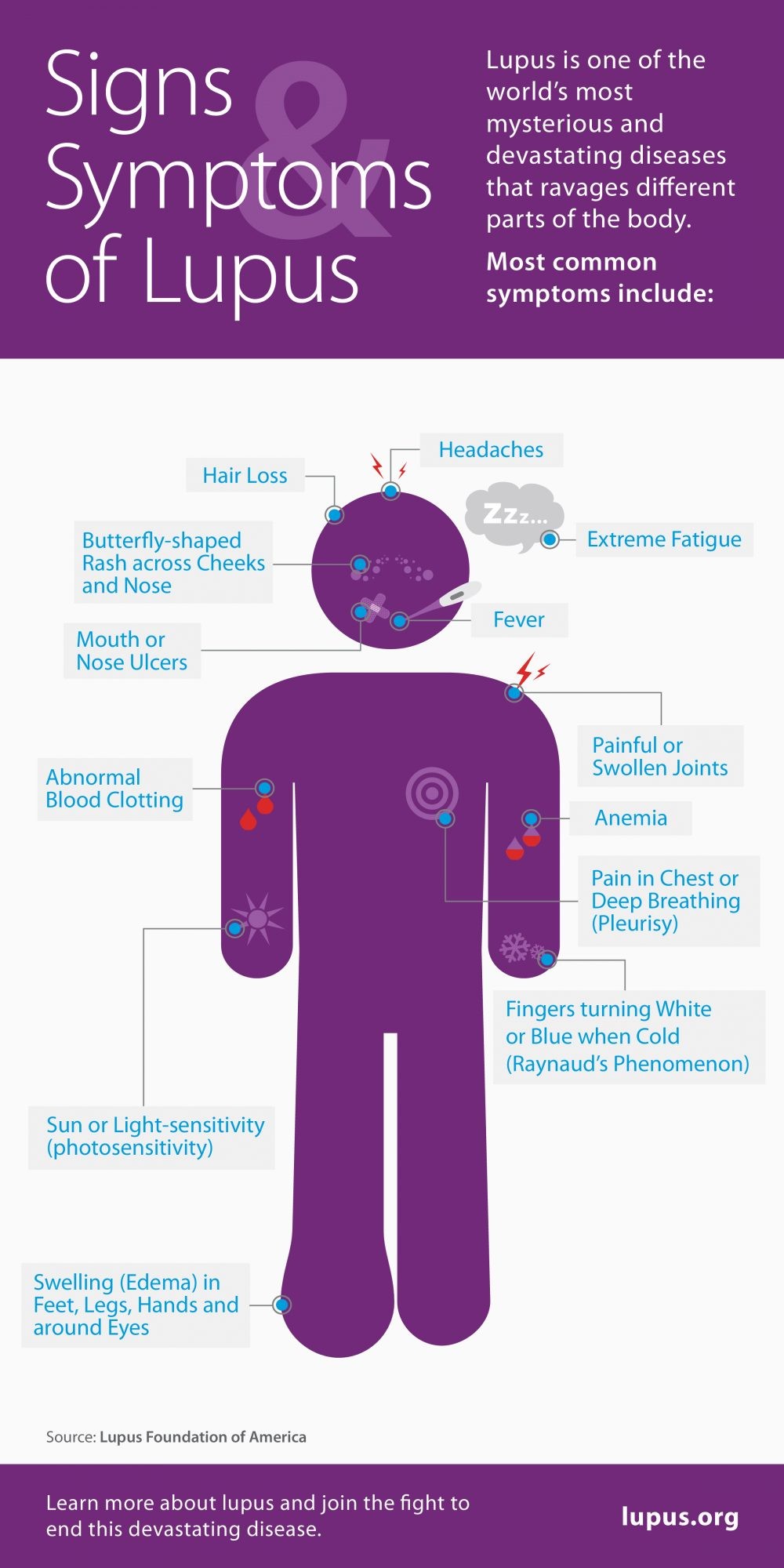
Symptoms
Frustration and misdiagnosis come from the fact that Lupus looks different for different people with measurable diagnostic metrics available in a blood draw.
- Pericarditis or pleuritis, an inflammation of the lining of the heart or an irritation of the lung tissue causing pain and/or shortness of breath.
- Sjogren’s Syndrome which affects moisture producing glands primarily in the eyes or mouth and characterized by fatigue. Sjogren’s can also confuse issues by being either a primary diagnosis or secondary to Lupus itself. Tennis great, Venus Williams has Sjogren’s Syndrome and has learned to manage the disease in order to continue competing as a professional athlete. 9 out of 10 people with Sjogren’s are women and most often post-menopausal.
- Other symptoms include fevers, fatigue, body and joint aches, skin lesions, headaches, shortness of breath, confusion, memory loss and a distinctive butterfly shape facial rash.
Risk Factors
While not exactly hereditary, a family history of Lupus may indicate a predisposition which can be triggered by outside elements. Women are 9 times more likely to have Lupus than men. Onset is often between age 15-44 but not always. Race and ethnicity can also play a role. African Americans, Hispanic, Asian American, Pacific Islander and indigenous Americans seem to have a higher incidence.
Triggers
Infections like influenza or Covid-19 can initiate or aggravate Lupus. People with Lupus experience higher degrees of photosensitivity. This makes them more susceptible to UV exposure causing rashes, fatigue, joint pain and other inflammation. Say ‘good-bye’ to sunbathing and ‘hello’ to lots of sunscreen! Different medications can initiate or aggravate Lupus like those for high blood pressure, seizures and some antibiotics. Drug related Lupus often dissipates after discontinuing those medications.
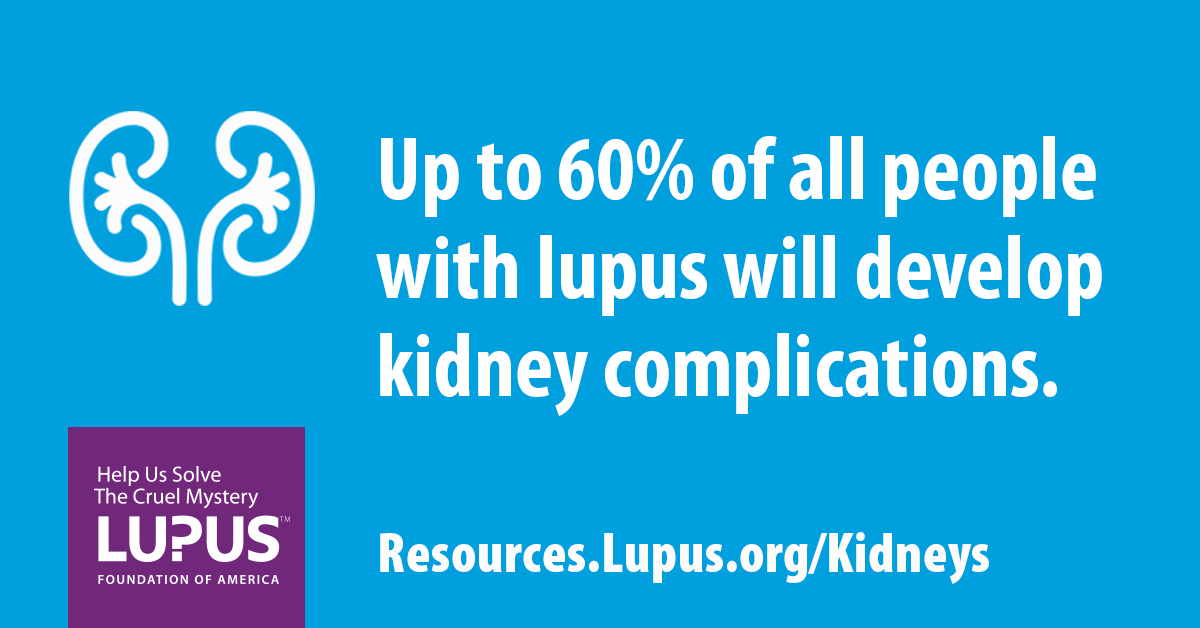
Complications
These are as varied as the symptoms and women with Lupus are 50 times more likely to suffer these complications.
- Kidney damage and failure are the #1 cause of death for Lupus sufferers.
- Brain/Central Nervous System problems. Headaches, memory loss, confusion, behavior changes, stroke, seizures, vision problems and difficulty expressing thoughts are all possible.
- Blood/blood vessels, anemia, an elevated risk for bleeding or clotting and inflammation of the vessels themselves.
- There is an elevated risk of pleural cavity inflammation, bleeding and pneumonia.
- There is an elevated risk of heart muscle, arterial inflammation, cardiovascular disease and heart attack.
Treatments and Lifestyle Adjustments
There are medications like Nonsteroidal anti-inflammatory drugs (NSAIDS) which can be used to reduce pain and inflammation. Anti-malarial drugs like hydroxychloroquine, corticosteroids like Prednisone and immunosuppressants like Methotrexate or Leflunomide have also proved effective. A healthy diet is important as well. Avoiding processed, preserved, salty and fried foods and including whole grains, fresh fruits, organic vegetables, lean meats, olive, sesame or flax seed oil are recommended. Regular exercise, weight control, stress reduction, vitamin D and calcium supplements, quitting smoking, sun protection and plenty of rest are lifestyle adjustments are healthy habits everyone should be observing and can help keep Lupus at bay.
80-90% of people with Lupus have a relatively normal life expectancy. Living with Lupus requires adjustments as it progresses in order to avoid ‘flare-ups’. Lifestyle changes are consistent with any other medical advice given for a normal and healthy life. Lupus requires you to become a vocal advocate for your own healthcare and lifestyle needs. Lupus is unpredictable. It can appear slowly or suddenly, be mild or severe, you can be young or old, male or female, be chronic or episodic plus the physical and mental pain is mostly invisible. Because you are in an internal war with your own body every morning is a ‘Lupus Lottery’ with what do we get today? Those of us with Lupus learn to be hyper-aware of our own body and our unique set of symptoms. As always, you learn to be your own healthcare advocate and work as a team with your rheumatologist and primary healthcare professionals. Nick Cannon says, “I have Lupus, but Lupus doesn’t have me.” Personally, I like ‘Hurdles are made to jump over.” Please join me on May 21, 2021 and wear purple for Lupus Awareness Day.
NHS Solutions provides Interim Nurse Leadership across a wide spectrum of healthcare specialties. Contact us if your organization is experiencing a leadership gap or seeks a change agent to step in with innovative techniques to transform a team in a short period of time. We have Interim Nurse Leaders available now in specialties such as neuroscience.